Introducing Avaneer Coverage Direct™, connecting payers and providers directly, avoiding intermediaries, and closing the gap left by existing solutions (EDI, clearinghouses, and portals).
Accurate coverage information is vital for payers and providers. Even if you already have coverage discovery tools, you may be missing coverage information due to the limitations of EDI, clearinghouses, and portals. Avaneer Coverage Direct™ provides payers and providers instant access to the latest coverage information.
Avaneer Coverage Direct includes the following features:
With Avaneer Coverage Direct, coverage information is refreshed daily and always available without having to call payers or search payer websites. The solution reveals misalignments and errors in payer and provider coverage information, allowing registration problems to be resolved upfront, streamlining patient access workflows.
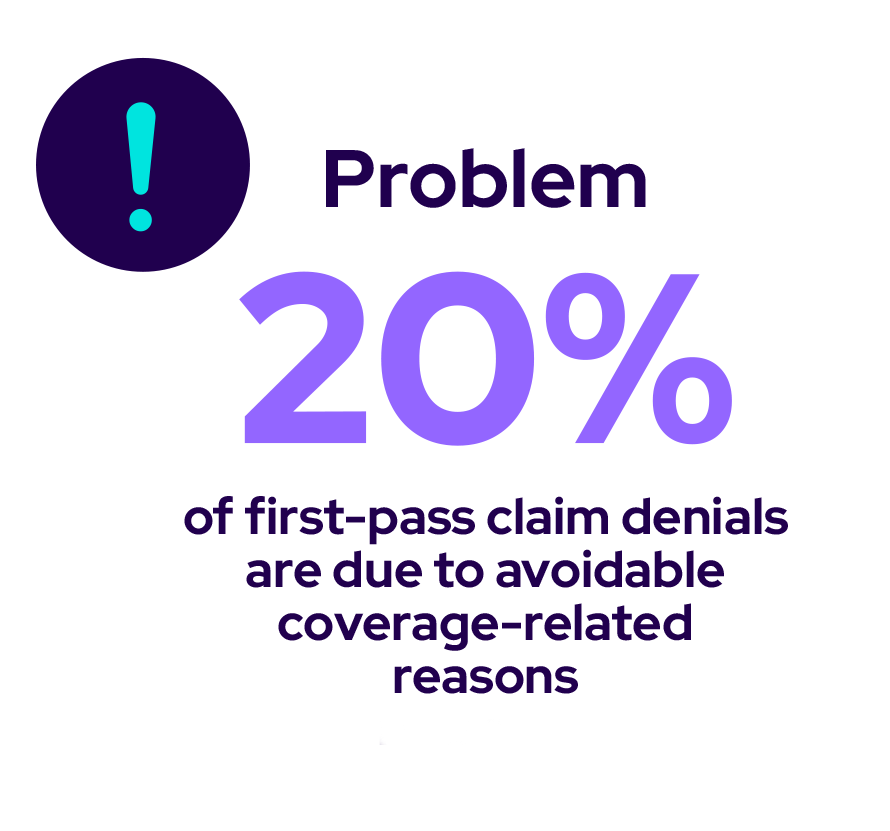
Avaneer Coverage Direct reduces



Every solution participant contributes patient/member data to their SparkZone™, their private environment on the Avaneer Network™, where Avaneer Coverage Direct evaluates each participant’s coverage information. Updated data is automatically pushed in real time to each participant’s source system so that corrections can be auto-posted and made available for use.
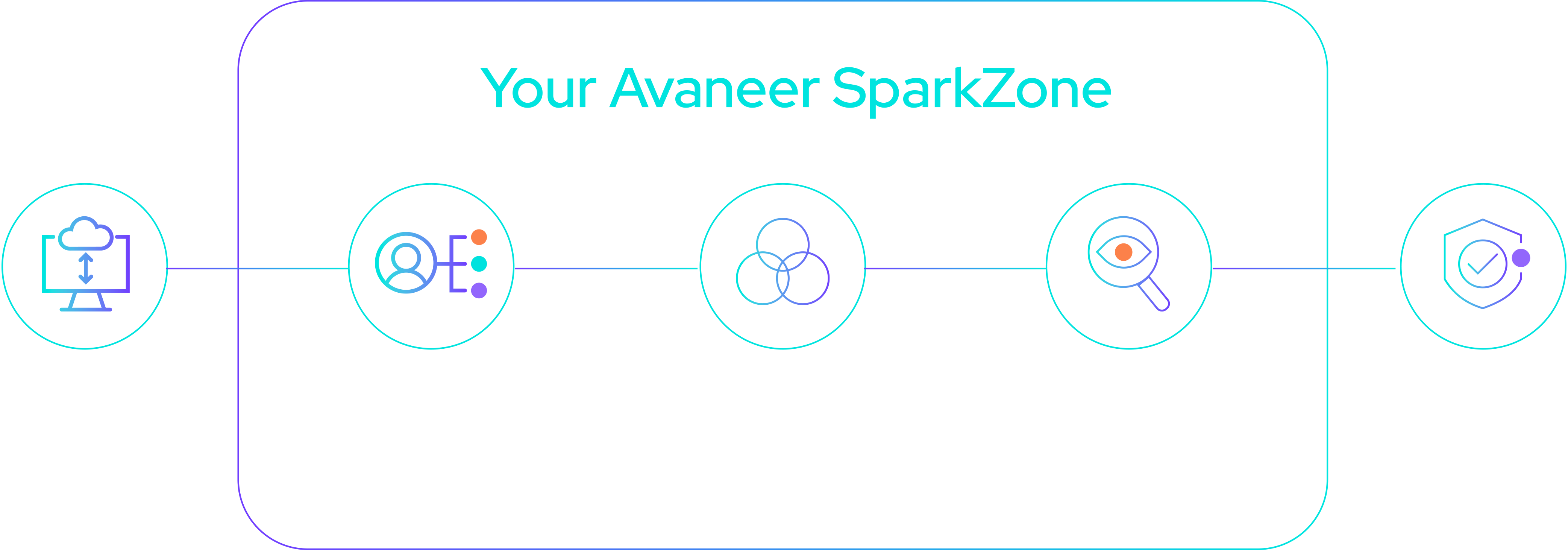
Coverage data is never aggregated and is shared directly between participants without third-party involvement.
Avaneer Coverage Direct gives providers and payers confidence that they always have the latest and most accurate coverage information in their source systems.
Payers lower administrative and operational costs and discover net-new COB opportunities beyond existing solutions.
Providers reduce denials, lower total cost of revenue cycle operations, and decrease write-offs.
Joining the network and using Avaneer Coverage Direct delivers administrative cost savings, improves member satisfaction, reduces provider friction, and creates an opportunity to seamlessly adopt upcoming solutions.

Having accurate coverage information is key to an efficient revenue cycle. Avaneer Coverage Direct delivers accurate, real-time coverage information directly from the payer's to the provider’s system. In addition to cost savings, providers can improve the patient experience and payer relations.

Introducing Avaneer Coverage Direct™, connecting payers and providers directly, avoiding intermediaries, and closing the gap left by existing solutions (EDI, clearinghouses, and portals).
Bob Gross, Executive Director of Financial Decision Support and Analysis at Cleveland Clinic, and Krista Matlock, Senior Director of Operations and Market Network Services at Cleveland Clinic, discuss value-based care.
Instead of continuing to add fixes on top of a broken system, healthcare needs to create a new, better system built with a new kind of interoperability to pave the way for a patient-centered healthcare ecosystem.