Strategic Guidelines for Getting Started with FHIR
In today's rapidly evolving healthcare landscape, the ability to securely and efficiently exchange patient data is paramount. The Fast Healthcare Interoperability Resources (FHIR) standard has emerged as a powerful tool to address this challenge. By providing a common language for healthcare data, FHIR enables seamless interoperability between different systems and organizations.
What is FHIR?
FHIR is a comprehensive framework that includes a set of data structures, elements, and APIs designed to support the exchange of electronic health records (EHRs) and other healthcare information. It offers a flexible and extensible framework that can accommodate a wide range of use cases, from clinical decision support to population health management.
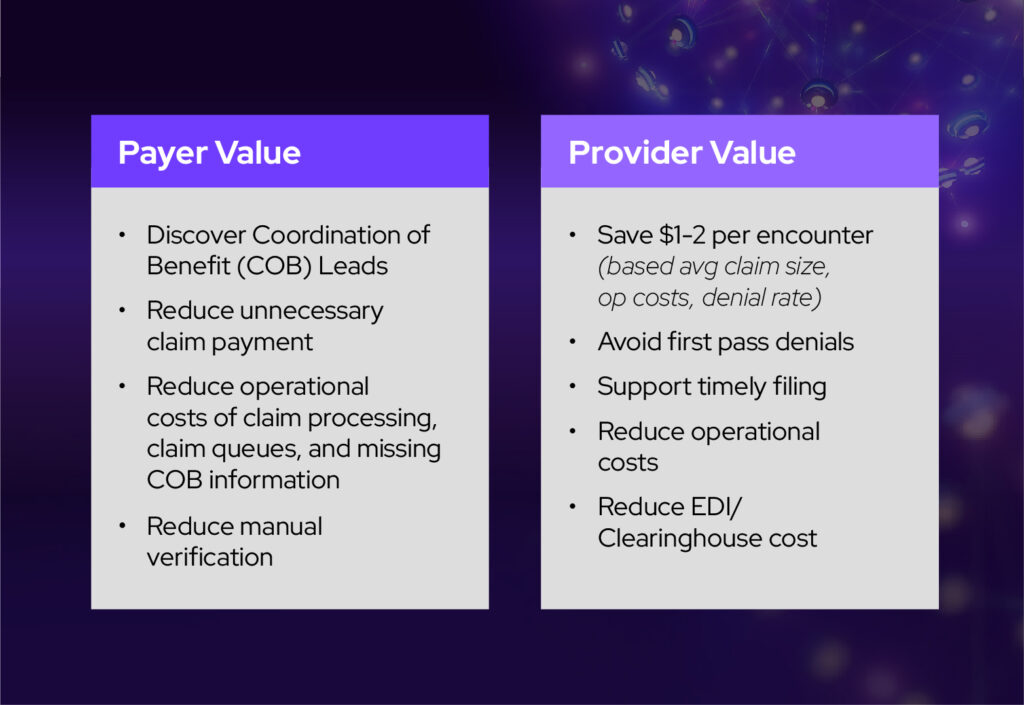
Getting Started: A Guide for Providers and Payers
The journey to adopting FHIR can seem daunting, but with the proper guidance, it can be a rewarding experience. Below are key steps that can help providers and payers get started.
Providers
- Assess your needs. Determine the specific use cases for FHIR within your organization. Are you looking to improve care coordination, streamline billing processes, enable patient-centric care, or all of the above?
- Leverage existing resources. Explore the wealth of resources available online, including the HL7 website and FHIR communities. These platforms offer tutorials, documentation, and best practices.
- Consider partnering. If you don't have the internal resources to build and maintain a FHIR server, consider partnering with a technology provider like Avaneer Health. We specialize in FHIR-based interoperability solutions that can help you exchange FHIR data with your trading partners.
Payers
- Understand regulatory requirements. Stay informed about the latest regulatory mandates related to healthcare data exchange. FHIR can play a crucial role in meeting these requirements. There are several online resources, such as CMS.gov and HealthIT.gov.
- Prioritize interoperability with your providers. Identify key areas where interoperability is most critical for your organization. You will likely have to meet your providers where they are on their FHIR journey to support many of your exchange needs. Leveraging a platform like the Avaneer Health Network can help you do just that.
- Invest in FHIR Technology. Explore FHIR-enabled platforms and tools that can help you streamline data exchange and improve operational efficiency.
Key Considerations for Adopting FHIR
As you embark on your FHIR journey, there are several vital factors to keep in mind, which include the following:
Regulatory Compliance
Why it matters. Adherence to regulatory standards is essential to avoiding penalties and maintaining patient trust. FHIR can help organizations comply with regulations like HIPAA and CMS mandates.
Considerations. Stay current with the latest regulatory requirements to ensure your FHIR implementation plan aligns with these standards. You may want to consider consulting with legal experts to understand your specific obligations.
Data Quality
Why it matters. High-quality data is crucial for accurate decision-making and effective care delivery. Inconsistent or inaccurate data can lead to errors, inefficiencies, and poor outcomes. However, disparate organizations can read and interpret the specifications differently, making it vital to collaborate and ensure alignment/understanding of the data values that populate the data elements.
Considerations. Establish data quality standards and implement processes to ensure data accuracy, completeness, and timeliness. Consider using data validation tools and techniques to identify and correct errors. A platform like the Avaneer Health Network can act as an intermediary to ensure that there is a shared understanding between participants regarding data exchange.
API Readiness
Why it matters. Deploying a FHIR server provides the required APIs, but your organization’s infrastructure and systems must be prepared to fully leverage them. Efficient API performance and system integration are key to ensuring smooth data exchange and interoperability.
Considerations. Evaluate your organization's network capacity and system readiness to support real-time FHIR interactions. Ensure that internal systems and external partners can successfully interact with the FHIR server's API endpoints. This includes verifying the capability of your IT environment to manage the expected volume of API requests and responses, as well as the ease of integrating with other existing healthcare systems.
Security & Privacy
Why it matters. Protecting patient data is a top priority. A breach of sensitive information can have serious consequences, both legally and reputationally.
Considerations. Implement robust security measures to protect FHIR-based systems and data. This not only involves the use of appropriate encryption, access controls, and security governance but also leveraging modern technology and architectural approaches to minimize risk.
Customization
Why it matters. While the FHIR standard is flexible, it may not align perfectly with your organization's specific needs. Customization can help ensure those needs are met. However, this can lead to data interoperability issues, as highlighted in the data quality section above.
Considerations. Identify areas where customization is necessary and carefully consider the implications of making changes to the standard. Involve subject matter experts and technical teams to ensure that customizations are implemented effectively.
Conclusion
FHIR-based data exchange continues to be at the forefront for addressing the challenges of healthcare interoperability. By understanding the fundamentals of FHIR and following the strategic approach outlined above, providers and payers can leverage this technology to improve patient care, enhance operational efficiency, and drive innovation in the healthcare industry.
Learn how your organization can partner with Avaneer Health for FHIR implementation